Your brain deserves better than mystery meat and butter by the pound. A study published in Neurology Open Access, a journal of the American Academy of Neurology, followed more than 100,000 women for over two decades and found that a Mediterranean-style eating pattern was linked to a lower risk of stroke.
It’s not a miracle. It’s a smarter default: olive oil instead of heavy fats, fish more often than processed meat, and vegetables that actually show up on your plate.
If your meals have turned into “whatever’s quick,” this is an easy upgrade that doesn’t feel like punishment. The Mediterranean approach isn’t about strict rules or perfect prep.
It’s about small swaps you can repeat without thinking, until they start working in your favor.
1. Risk Reduction Isn’t a Force Field
Let me clear something up right now. A 25% lower risk sounds fantastic, and it is, but it doesn’t mean you’re suddenly immune to strokes.
The strongest benefit showed up for hemorrhagic strokes, the kind where bleeding happens in your brain, and yes, that 25% drop is impressive.
But here’s the thing. Risk reduction is not the same as a get-out-of-jail-free card.
You can eat like a Greek islander and still have other risk factors at play.
Think of it this way: lowering your risk by a quarter is like shaving a quarter off your grocery bill every week. It adds up, it matters, but you’re not shopping for free.
The diet helps stack the odds in your favor, especially over the long haul, but it works best when combined with other healthy habits like staying active and not smoking. So celebrate the win, but keep your expectations realistic and your lifestyle well-rounded.
2. All Stroke Types Got Some Love
Here’s where it gets even better. The Mediterranean diet didn’t just help with one type of stroke.
It showed benefits across the board, which is rare and worth celebrating.
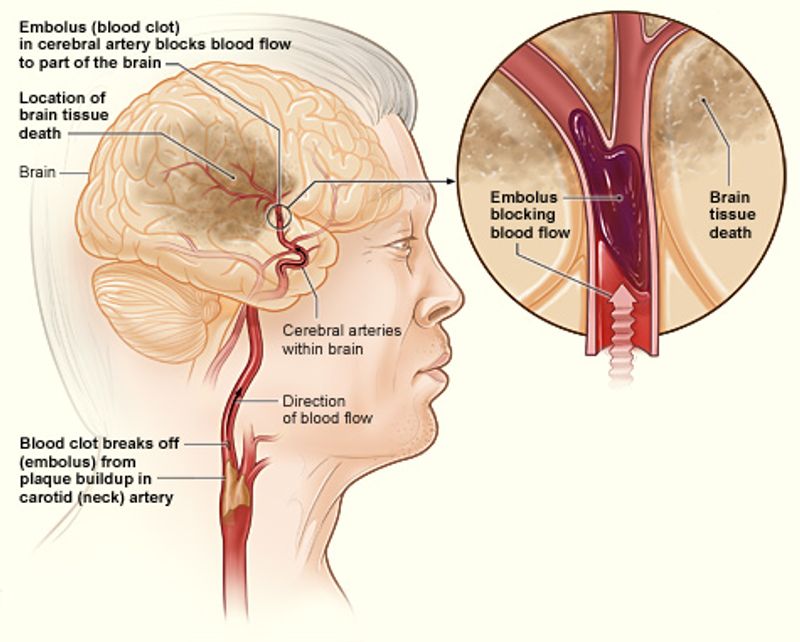
The study found an 18% lower likelihood for all strokes combined. Ischemic strokes, the most common kind caused by blockages, dropped by 16%.
And hemorrhagic strokes, the less common but often nastier ones, saw that headline-grabbing 25% reduction.
That’s a pretty solid trifecta. Most diets show mixed results depending on the condition, but this eating pattern seemed to offer broad protection.
It suggests that the combination of foods, rather than any single ingredient, creates a ripple effect throughout your vascular system. Whether it’s keeping arteries clear or managing blood pressure, the Mediterranean approach appears to work on multiple fronts.
So you’re not just protecting against one threat, you’re building a more resilient system overall.
3. Two Decades of Real-Life Data
Anyone can stick to a diet for a month. Heck, I once ate nothing but smoothies for two weeks and felt like a health guru.
Then reality hit and I was back to pizza by week three.
This study followed participants for about 21 years. That’s not a trendy cleanse or a New Year’s resolution that fizzles by February.
That’s real life, with all its ups, downs, holidays, and stressful Tuesdays.
The long follow-up period makes the findings much harder to dismiss. Short-term studies can be skewed by temporary changes or the placebo effect of feeling virtuous.
But over two decades, patterns emerge that reflect actual sustained habits and their true impact on health. It also means the researchers could track outcomes that take years to develop, like strokes, which don’t usually pop up overnight.
So when the data shows benefits after that much time, it carries serious weight.
4. Big Numbers, Specific Group
The research team tracked 105,614 women living in California. That’s a massive sample size, which is fantastic for statistical power.
Average age at the start was 53, and none had experienced a stroke before joining the study.
So the dataset is strong and the numbers are solid. But here’s the catch: it was women only, mostly in one geographic area, and within a certain age range.
That doesn’t automatically mean the results won’t apply to men, younger people, or other populations, but it does mean we should be a bit cautious about overgeneralizing.
Different groups can respond differently to dietary patterns based on genetics, environment, and cultural food habits. The findings are still valuable and point in a promising direction, but they’re not a one-size-fits-all guarantee.
More research including diverse populations would help confirm whether the benefits hold up across the board. For now, it’s a strong signal, not a universal law.
5. Patterns Trump Single Superfoods
Forget hunting for the one magic ingredient that will save your brain. Spoiler: it doesn’t exist.
What mattered in this study was the overall eating pattern, not whether you ate three extra blueberries on Tuesday.
Participants scored higher when they regularly ate the core Mediterranean staples and avoided the foods that pattern typically limits. It’s the combination and consistency that count, not isolated nutrients or trendy superfoods.
One serving of salmon won’t undo a diet heavy in processed junk, and a handful of almonds can’t compensate for skipping vegetables entirely.
The Mediterranean diet works because it creates a synergy. Olive oil provides healthy fats, fish delivers omega-3s, vegetables and fruits bring fiber and antioxidants, and whole grains keep blood sugar steady.
Together, they support vascular health in ways that no single food can replicate. So stop looking for shortcuts and start thinking about your plate as a whole ecosystem.
6. The Scoring System Rewarded These Stars
Participants earned points for eating above-average amounts of specific foods. The list reads like a greatest hits album of nutrition: whole grains, fruits, vegetables, legumes, olive oil, and fish.
Notice what’s missing? Processed snacks, sugary drinks, and mystery meats.
The scoring system wasn’t about perfection. It was about eating more of the good stuff more often.
If your intake of these core foods was higher than the average person’s, you scored points. Simple as that.
This approach makes the diet more accessible because it’s not about strict rules or eliminating entire food groups overnight. You don’t need to eat kale at every meal or never touch bread again.
You just need to make these staples a regular part of your routine. The more consistently they show up on your plate, the better your score, and apparently, the lower your stroke risk.
It’s a flexible framework, not a rigid prison.
7. Moderation Got Credit Too
The scoring system included moderate alcohol intake as part of the Mediterranean pattern. Before you pop a bottle of wine and call it health food, let’s pump the brakes.
This doesn’t mean drinking is required or even recommended.
The key word here is moderation, and the nuance is important. The traditional Mediterranean lifestyle often includes a glass of wine with meals, but it’s not the hero of the story.
The study’s scoring system counted it because it’s characteristic of the pattern, not because alcohol itself is a health tonic.
If you don’t drink, don’t start because of this study. If you do drink, keeping it moderate is the point.
Heavy drinking increases stroke risk, so there’s a fine line here. The takeaway is that the diet pattern as a whole, including moderate habits around alcohol, was associated with benefits.
It’s about balance and context, not a free pass to overindulge.
8. Less of the Usual Suspects
Participants scored better if they ate less red meat and fewer dairy products than the average person. Notice the study didn’t say eliminate them entirely.
It’s about eating less, not living in deprivation.
In practice, this often means replacing rather than just removing. Swap that steak for grilled fish a few nights a week.
Trade butter for olive oil in your cooking. Use yogurt sparingly instead of loading up on cheese at every meal.
The Mediterranean approach isn’t about demonizing food groups. It’s about shifting the balance so that plant-based foods, fish, and healthy fats take center stage, while red meat and heavy dairy become supporting actors.
That shift, sustained over time, seems to make a difference for vascular health. You’re not giving up flavor or satisfaction, you’re just rearranging the lineup on your plate.
And your arteries will likely thank you for it.
9. Simple Swaps Beat Overnight Overhauls
Trying to flip your entire diet overnight is a recipe for burnout. I’ve seen people go from fast food to full Mediterranean zealot in 24 hours, only to crash and burn by the weekend.
Slow and steady wins this race.
Instead of a dramatic transformation, focus on simple swaps. Use olive oil instead of butter when you cook.
Grab a handful of nuts or a piece of fruit instead of processed snacks. Eat fish or legumes more often, and save red meat for occasional meals rather than daily staples.
These small changes add up without feeling like punishment. You’re not overhauling your life, you’re just tweaking your defaults.
Over time, those tweaks become habits, and those habits become your new normal. The beauty of the swap strategy is that it’s sustainable.
You’re building a pattern that fits into real life, not a rigid plan that requires superhuman willpower. And that’s exactly what the long-term study participants did, whether they realized it or not.
10. Why It Might Work: Vessels and Pressure
The study controlled for major stroke-related factors like smoking, physical activity, and high blood pressure. Even after accounting for those heavy hitters, the Mediterranean diet pattern was still linked to lower stroke risk.
That’s a big deal.
It suggests the diet itself is doing something beneficial beyond just being part of a generally healthy lifestyle. The likely mechanisms involve blood vessel health and blood pressure management.
Olive oil and fish provide fats that support flexible, resilient arteries. Vegetables and fruits deliver potassium and antioxidants that help regulate blood pressure.
Whole grains and legumes keep blood sugar stable, which protects vessel walls from damage over time. Together, these foods create an environment where your cardiovascular system can function smoothly.
It’s not magic, it’s physiology. The diet works with your body’s natural processes to keep blood flowing where it should, without the blockages or ruptures that cause strokes.
And that’s a win worth celebrating.
11. Hemorrhagic Strokes Are Rare but Brutal
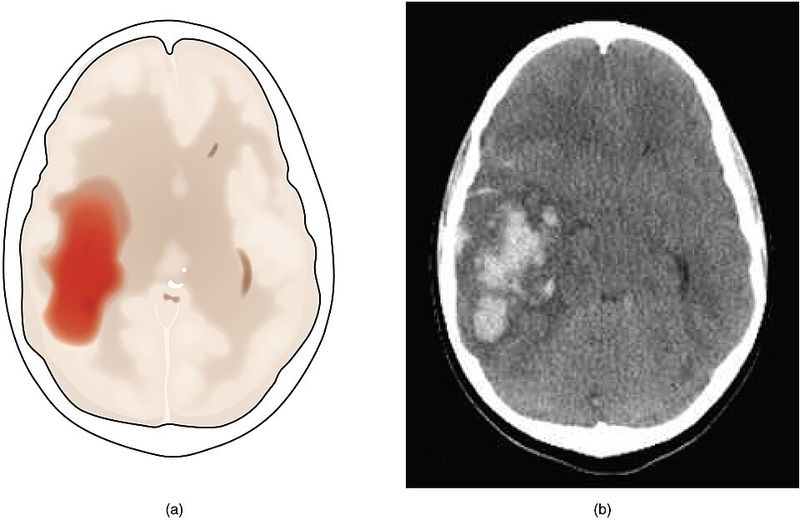
Hemorrhagic strokes are less common than ischemic strokes, but when they happen, they’re often much more serious. They involve bleeding in the brain, which can cause rapid and severe damage.
Survival rates are lower, and recovery is often harder.
That’s why it’s so encouraging that the strongest association in this study was with hemorrhagic stroke. A 25% lower risk for the most dangerous type is a quiet but powerful win.
It suggests the Mediterranean diet might offer protection where it’s needed most.
The mechanisms likely involve blood pressure control and vessel integrity. Chronic high blood pressure weakens blood vessel walls, making them more prone to rupture.
A diet rich in potassium, healthy fats, and antioxidants helps keep pressure in check and vessels strong. While ischemic strokes get more attention because they’re more common, reducing hemorrhagic stroke risk is equally, if not more, important.
Every percentage point of protection counts when the stakes are this high.
12. Association, Not Proof
Here’s the part where I put on my science hat. The study found a link between Mediterranean eating and lower stroke risk, but it did not prove that the diet causes the reduction.
That’s a critical distinction.
This type of research is observational, meaning it tracks people over time and looks for patterns. It can’t control every variable the way a randomized controlled trial can.
Maybe people who eat Mediterranean-style also walk more, stress less, or have better social support. Those factors could play a role too.
That said, observational studies are valuable, especially for long-term outcomes like stroke. You can’t ethically randomize people to eat poorly for 21 years just to see what happens.
The association here is strong, consistent, and backed by plausible biological mechanisms. So while we can’t say the diet definitely causes lower stroke risk, the evidence is compelling enough to take seriously.
It’s the best we’ve got, and it points in a very promising direction.
13. Real Limitations That Matter
Every study has limitations, and this one is no exception. Two big ones stand out: only women were included, and diet was self-reported.
Both matter when interpreting the results.
The women-only focus means we can’t automatically assume the same benefits apply to men. Hormones, metabolism, and cardiovascular risk profiles differ between sexes, so the effects might not be identical.
More research including men is needed to confirm whether they see similar protection.
Self-reported diet data is notoriously imperfect. People forget what they ate, underestimate portion sizes, or report what they think they should be eating rather than what they actually consume.
That can introduce error into the findings. Despite these limitations, the study’s size, duration, and consistent results give it weight.
The limitations don’t erase the findings, they just remind us to interpret them carefully and look forward to future research that fills in the gaps.
14. Your Default Plate Matters Most
Forget complicated rules and calorie counting. The practical takeaway is simple: change your defaults.
If your typical plate is half vegetables, uses olive oil as the main fat, includes nuts or legumes regularly, features fish fairly often, and treats red meat as an occasional guest rather than a daily staple, you’re already living the pattern.
This isn’t about perfection or never enjoying a burger again. It’s about what shows up most often.
Your defaults shape your long-term health more than any single meal or occasional indulgence. If the Mediterranean staples become your go-to choices, you’re aligning with the eating pattern linked to lower stroke risk in this research.
Start small if you need to. Add an extra serving of vegetables today.
Cook with olive oil tomorrow. Swap in fish next week.
Over time, those small shifts become your new normal, and your new normal could mean better odds for your brain and your future.